Are administrative challenges limiting your healthcare practice’s efficiency? Medical billing is a crucial yet intricate process. Roughly 30% of medical practices report claim denials due to medical coding errors or delays.
For many healthcare organizations, outsourcing medical billing services has become a practical solution to alleviate administrative burdens, improve claim accuracy, and allow greater focus on patient care.
In this guide, we’ll explore the many benefits of outsourcing medical billing services, examine the challenges to consider, and offer insights to help you determine if this approach fits the needs of your medical practice.
READ MORE: What is Healthcare BPO & How Healthcare Providers Can Use It
What is Medical Billing Outsourcing?
Medical billing outsourcing involves contracting an external company to handle claim submission, payment processing, and overall revenue tracking. This service provides medical practices with access to trained medical billing experts and reduces the complexities of in-house billing. Outsourcing has proven effective, with industry research suggesting it can reduce billing errors by up to 80% and help practices recover 15% more revenue on average.
Billing companies frequently use advanced technologies, including automated billing systems and real-time tracking tools, further streamlining processes. Studies indicate outsourced billing can reduce denial rates by 10–20%, enhancing cash flow and allowing practices to focus more on core functions and treatment of patients.
Medical Billers vs. Medical Coders
Medical billers and medical coders play distinct roles in the healthcare revenue cycle. Medical billers handle claim submissions, manage collections, and follow up on denials. Their focus is on optimizing revenue flow, working with insurers, and addressing patient billing inquiries. They require strong communication skills and knowledge of insurance guidelines.
In contrast, medical coders translate medical diagnoses and procedures into standardized codes like CPT, ICD, and HCPCS. This ensures accurate documentation and compliance for billing. Coders need precision and expertise in medical terminology and coding systems.
Pros and Cons of Outsourcing Medical Billing Services
Outsourcing medical billing offers cost savings, efficiency, and scalability, but practices should also consider potential challenges like reduced oversight and dependency on external providers.
Outsourced Medical Billing Benefits
- Save Money: Outsourcing medical billing eliminates the need to hire and manage an in-house billing team, which reduces expenses associated with recruitment, training, and retention of skilled personnel. This approach also minimizes overhead expenses, providing healthcare practitioners with a more budget-friendly option for managing their billing workload.
READ MORE: Reducing Operational Costs Through Remote Work & Outsourcing
- Efficiency Boost: Professional billing teams have specialized knowledge of billing codes and procedures, ensuring that claims are accurately filed on the first attempt. This expertise helps mitigate common claim errors and rejections, which can hinder revenue cycles and result in unpaid claims. When you outsource medical billing services to a dedicated team, your medical facility can experience faster claim submissions, shorter payment cycles, and a noticeable increase in revenue.
- Focus on Patient Care: When healthcare organizations outsource medical billing, in-house staff can dedicate more time and energy to patient-centered activities. This shift enables medical teams to allocate resources toward improving patient experiences and outcomes, fostering a more rewarding and efficient practice environment.
- Scalability: Outsourcing medical billing allows healthcare practices to easily scale operations up or down, adjusting to fluctuations in patient volume or growth. Billing companies provide flexible solutions that can evolve alongside a practice, ensuring efficient billing processes without the need for permanent medical billing staff.
- Access to Expertise: Medical billing companies are well-versed in current industry standards, insurance regulations, and compliance requirements. They stay updated with new billing codes, laws, and best practices, minimizing the risk of claim rejections or compliance penalties. Partnering with an expert billing provider provides peace of mind, knowing your billing is managed by skilled professionals who prioritize accuracy and regulatory adherence.
Challenges of Outsourced Billing Services and How to Overcome Them
- Data Security Concerns: Transferring sensitive information to an external provider can introduce data security risks, as protecting patient confidentiality under HIPAA becomes more complex. Partner with a medical billing company that prioritizes data security as HIPAA-compliant and employs advanced cybersecurity protocols, like encrypted storage, secure data transfer, multi-factor authentication, and regular security audits.
- Loss of Direct Oversight: Outsourcing may limit control over daily billing tasks, making monitoring the accuracy and speed of claim processing harder. Establish clear service level agreements (SLAs) and set up regular communication checkpoints with the provider. Access to real-time reporting or billing dashboards further lets you stay informed about billing progress, keeping you connected to important performance metrics.
- Initial Adjustment Period: Transitioning to outsourced billing can briefly disrupt workflows and require time for staff to adapt. Work with a provider that offers a structured onboarding process, ensuring smooth transfers and familiarizing your team with the new procedures. Many billing companies also provide initial training to help your staff build confidence and quickly adjust to the new system.
- Dependency on External Provider: Relying fully on an external company for billing can lead to dependency, potentially complicating transitions if the service declines. Choose a provider with a reliable reputation and create a contingency plan that details steps to seamlessly switch providers if needed.
READ MORE: 7 Outsourcing Myths Holding Back Your Business Growth
Key Considerations When Outsourcing Billing Services
Deciding whether to outsource medical billing involves assessing various factors:
Billing Complexity and Volume
Consider the complexity of your billing needs and the volume of claims. Specialty practices or those with high claim volumes may benefit more from outsourcing, especially if the billing codes involved are complex and prone to errors.
Cost and ROI
Compare outsourcing medical billing expenses with the cost of an in-house dedicated medical biller team, including payroll, training, and software costs. Outsourcing can offer a strong ROI by reducing billing mistakes, claim denials, and overhead costs.
Data Security and HIPAA Compliance
Data security is critical for all healthcare services and organizations. Choose providers with stringent data protection measures and HIPAA compliance, verified through third-party certifications or regular security audits.
Service Level Agreements SLAs
Set clear SLAs with your billing partner to define standards for performance metrics, such as claim submission timelines, accuracy, denial management, and reporting.
Reputation and Expertise in Your Specialty
Partner with a billing provider with a strong track record, particularly one with experience in your medical specialty. This ensures they are familiar with the nuances of your billing codes and processes.
Communication and Support Availability
For efficient and effortless outsourced medical billing services, look for a billing company with responsive communication and reliable customer support, including real-time reporting options to keep you updated on claim statuses and billing metrics.
Scalability and Adaptability
Confirm that the outsourcing billing company can scale its services as your medical practice grows or patient volumes shift, allowing billing support to expand or contract without disrupting operations.
Transition Planning
A clear transition plan helps mitigate workflow disruptions. Collaborate with your outsourcing partner on secure data transfer methods and training to familiarize your team with new systems.
READ MORE: 9 Top Outsourcing Countries
Outsourcing Medical Billing vs In-House Medical Billing
Outsourcing versus in-house medical billing is a crucial decision for healthcare practices, each option offering unique benefits and challenges. Outsourcing typically involves per-claim or percentage-based fees, allowing flexibility aligned with revenue, while in-house billing incurs fixed costs such as salaries, training, and software maintenance.
Outsourcing also provides access to specialized billing experts skilled in coding, compliance, and denial management, which can reduce errors and boost revenue. In contrast, in-house teams offer direct control but may struggle to stay updated with regulatory changes, risking billing inaccuracies.
Scalability is another advantage of outsourcing. As patient volumes fluctuate, an outsourced provider can adapt without requiring the practice to hire or train more staff. In-house billing, however, demands significant resources for scaling, including recruitment and management, which can become a time-intensive process.
Outsourcing also alleviates the administrative burden on healthcare providers, freeing up time for patient care. This can enhance patient treatment, as providers focus on delivering a quality experience without being sidetracked by billing. In-house billing, while closer to practice operations, may demand additional staff attention and resources, potentially impacting patient interactions.
| Outsourced Medical Billing | In-House Team | |
| Cost Structure | Flexible per-claim or percentage fees, adjusting with revenue. | Fixed costs for salaries, training, and software, which are potentially burdensome. |
| Expertise | Access to specialists in coding, compliance, and denial management, minimizing errors. | Direct control, but may lack advanced billing knowledge. |
| Scalability | Easily adjusts to patient volume without new hires. | Scaling requires recruiting and managing more staff, consuming time. |
| Patient Satisfaction | Reduces administrative tasks, allowing more patient-focused time. | Direct oversight can divert resources, impacting patient satisfaction. |
Current Trends in Medical Billing and Why They Matter
According to industry research, approximately 75% of healthcare facilities are exploring outsourced medical billing as a strategic solution to meet the demands of the healthcare industry.
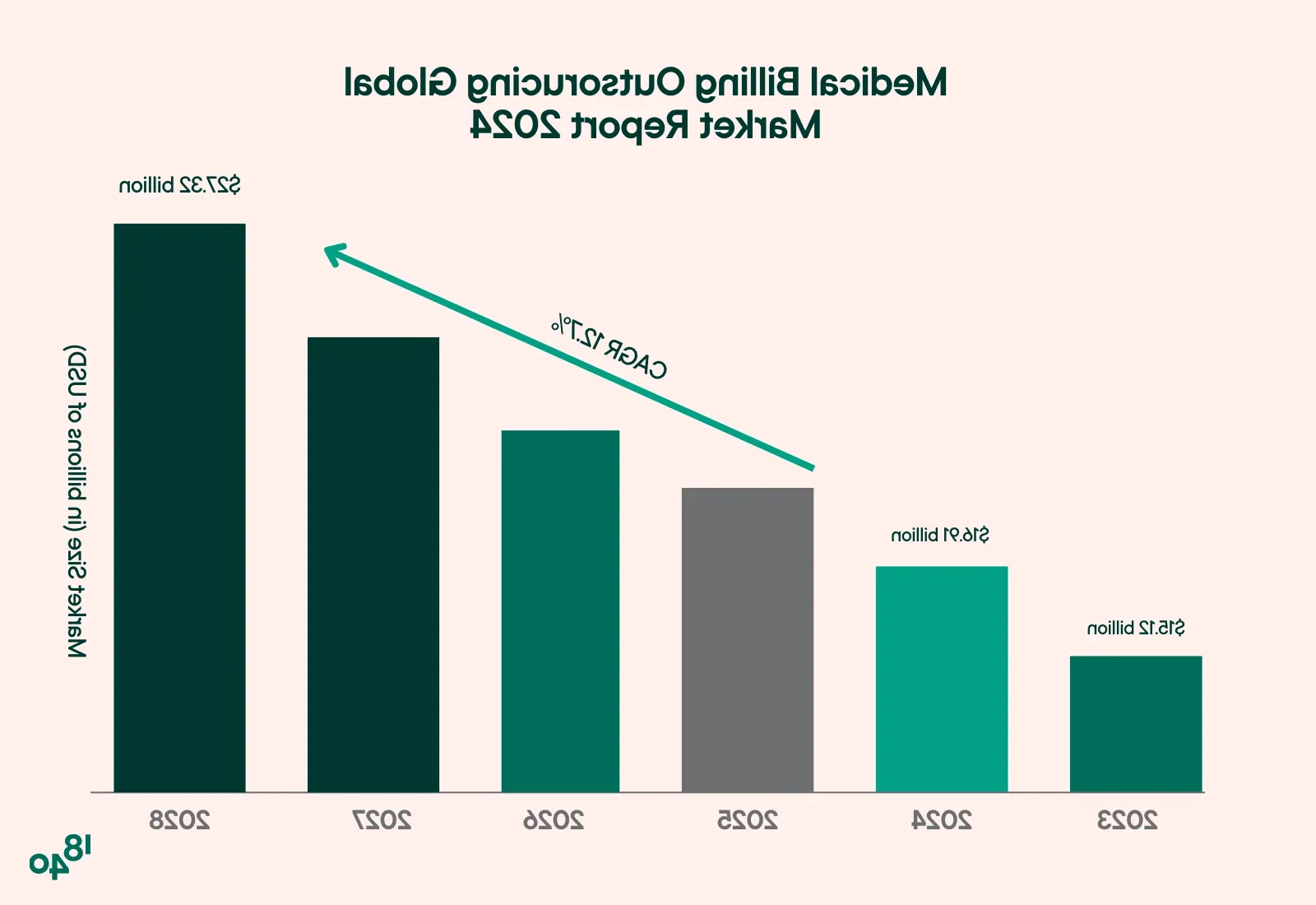
The medical billing outsourcing market has grown by 12% over the past two years as practices aim to reduce billing costs, improve collections rates, and shorten payment cycles.
Key industry trends driving this shift include:
- Increasing Billing Complexity: As healthcare regulations and insurance protocols grow more complex, practices need to stay compliant and up-to-date. Outsourced billing providers offer the specialized knowledge needed to navigate these changes.
- Enhanced Data Security Needs: HIPAA compliance and cybersecurity are non-negotiable in healthcare, but maintaining in-house compliance can be costly. Many outsourced providers include compliance and security in their services, easing this burden on practices.
- Focus on Patient-Centered Care: With the administrative side of the practice handled externally, providers can focus more on patients and less on the details of billing, offering better patient outcomes and satisfaction.
By 2028, the global outsourced medical billing market is expected to reach approximately $27.3 billion, reflecting a strong growth trend.
How to Outsource Medical Billing
Outsourcing medical billing effectively requires evaluating your practice’s needs, selecting a reputable provider, and establishing clear performance expectations to ensure a smooth transition and ongoing success.
Assess Your Practice’s Needs
Identify specific goals and challenges in your current billing process. Determine which tasks (e.g., claim submission, follow-ups, reporting) would benefit most from outsourcing. Understanding your practice’s billing volume, common pain points, and revenue goals helps you select the right outsourcing billing partner and define expectations clearly.
Research Potential Providers
Look for billing companies with experience in your medical specialty, as well as a strong reputation for security, compliance, and results. Review case studies, client testimonials, and service offerings to ensure they align with your needs.
Evaluate Cost Structures and Service Packages
Medical billing companies offer a range of pricing models, from percentage-based fees to flat-rate packages. Compare pricing and services carefully to understand what’s included, like claim follow-ups, reporting, or patient support.
Establish Clear SLAs
SLAs define key expectations, such as claim submission timelines, accuracy rates, denial management, and reporting frequency. Setting these standards upfront provides a basis for performance monitoring and accountability.
Prioritize Data Security and Compliance
Ensure the provider has strong security protocols, such as encryption, secure data storage, and regular security audits, to safeguard patient information. Verify their HIPAA compliance and inquire about their employees’ training procedures.
Plan for a Smooth Transition
The shift to outsourcing may initially disrupt workflows, so work with your provider to create a transition plan that includes onboarding support and training for your staff. This might include setting up a secure billing data transfer, integrating the provider’s billing software with your practice’s system, and establishing regular communication channels.
Monitor Performance Regularly
Once the outsourcing process is underway, use reports and dashboards provided by your billing partner to monitor key performance indicators (KPIs), like claim acceptance rates, revenue cycle times, and outstanding receivables. Schedule regular meetings to review performance, discuss any issues, and make adjustments as needed to meet your practice’s financial goals.
Maintain Open Communication and Feedback Loops
Regularly communicate with your billing provider to discuss performance, address concerns, and align on future goals. A strong partnership involves ongoing feedback to ensure the provider adapts to your practice’s evolving needs. This proactive communication helps you maximize the benefits of outsourcing and ensures continuous improvement in your billing operations.
Key Performance Indicators (KPIs) for Outsourced Medical Billing Success
To ensure billing operations are efficient and effective, practices should regularly track specific KPIs, whether billing is managed in-house or outsourced. Focusing on these metrics can provide clarity on revenue cycle management performance and help identify areas for improvement:
- Claims Processing Time: This KPI measures the average time from claim submission to payment. Faster claims processing, ideally within 30 days, ensures steady cash flow. A high “first-pass claims rate” (the percentage of claims paid upon the first submission) also reflects efficient billing processes.
- Collections Ratio: This ratio indicates the percentage of total billed services collected. A strong collections ratio—ideally above 95%—demonstrates an effective billing process and minimal revenue loss due to denied or uncollected claims.
- Net Collection Rate: The net collection rate represents the percentage of revenue collected from all collectible charges. Practices should aim for a rate above 95% to reflect optimized revenue capture. This metric is a strong indicator of overall billing efficiency and the practice’s ability to convert billed services into revenue.
What to Look For in Outsourced Billing Companies
For many healthcare organizations, outsourcing medical billing raises questions about control, cost, and data security. However, reputable outsourced medical billing companies offer transparent reporting and communication, allowing you to monitor billing processes in real time.
- HIPAA Compliance: Ensuring the protection of patient data is non-negotiable. Seek a medical billing service provider with proven HIPAA-compliant practices, including data encryption, secure data storage, and routine security audits. HIPAA violations can lead to fines of up to $100,000 per year, per violation category, making compliance critical.
- Experience in Your Specialty: Billing for specialized medical fields requires niche knowledge of codes and regulations. A medical billing partner experienced in your specialty will better understand your billing complexities and improve claim accuracy.
- Transparency and Reporting: Opt for providers offering transparent reporting, real-time dashboards, and regular performance updates.
- Customizable Solutions: A flexible medical billing partner allows your billing processes to evolve with your practice. Data suggests that healthcare providers using customizable billing solutions report a 20% increase in operational efficiency over time.
- Support and Communication: Effective, responsive customer support is essential to address any issues promptly. Clear communication enables seamless collaboration, providing the reassurance that your billing is running smoothly.
READ MORE: Nearshore Vs. Offshore Outsourcing: Which is Better?
Why Choose 1840 and Company for Medical Billing Outsourcing?
At 1840 and Company, we leverage our extensive healthcare industry experience to deliver exceptional, customized services tailored to your needs.
Every healthcare practice faces unique challenges. Our healthcare outsourcing team specializes in providing HIPAA-compliant medical billing services that align with your operational demands. This personalized approach ensures effective solutions that resonate with the nuances of your practice.
We prioritize accuracy and compliance, training our billing specialists in the latest standards and industry regulations. This commitment helps maintain high accuracy rates in claim submissions and reduces the likelihood of denials, facilitating a smooth revenue cycle.
Recap: Is Medical Billing Outsourcing Right for Your Practice?
Outsourcing medical billing can transform how healthcare practices handle their revenue cycles—reducing costs, improving efficiency, and enhancing revenue predictability. By working with a specialized billing partner, practices can streamline operations, focus more on patient care, and reduce the complexities of in-house billing.
Ready to improve your practice’s billing process? Partnering with 1840 and Company gives you access to industry-leading expertise. Discover how we can help you optimize your billing operations—schedule a call today to explore how our services can support your practice’s growth and success.